__
WHO releases new tightened guidelines regarding the diagnostic criteria for COVID-19.
PCR positive no longer means you have COVID-19. You need a second test to confirm you have the virus | Tech News | Startups News
Yesterday, The World Health Organization released a new set of tightened guidelines and diagnostic criteria for detecting COVID-19 on the same day the 46th President of the United States was sworn in. The new guidelines may impact how healthcare professionals count the number of people infected with COVID-19.
The new tightened guidelines, which were released on January 20, were actually dated January 13. Call it coincidence or a chance, The WHO gave no reasons as to why the guidelines were delayed for one week before it was released.
The new guidelines involve the use of Nucleic acid testing (NAT) technologies that use polymerase chain reaction (PCR) for the detection of SARS-CoV-2. The WHO said the new guidelines “clarify information previously provided” by the organization.
Now according to the new WHO guidelines, a single positive PCR test for the virus isn’t going to cut it anymore. The fact that you are PCR positive no longer means you have COVID-19. In other words, you don’t have COVID-19 unless you get a second test to confirm it, and are presenting clinical symptoms. WHO also said that, even if you don’t show any symptoms, you’ll need to get a second test for confirmation as well.
In addition, The new WHO guidelines now demand that clinicians “must” also consider a wide array of other factors, like “timing of sampling, specimen type, assay specifics, clinical observations, patient history, confirmed status of any contacts,” and even something called “epidemiological information”—whatever that exactly is—before diagnosing anyone with COVID-19.
However, these tightened guidelines should not a surprise for anyone who has been following the organization. WHO is just returning back to what used to be the standard operating procedure. Before coronavirus hit in December 2020, neither WHO nor the CDC had ever considered a single positive PCR test sufficient for diagnosing viral infection.
Back in August, we wrote about how 90% of people who tested positive in 3 states barely carried coronavirus. Stunning new research also found that the usual COVID-19 PCR diagnostic tests may simply be too sensitive and too slow to contain the spread of the virus.
For example, in all four epidemics prior to COVID-19 since 2000, The CDC and WHO were concerned about the high false-positive rates for PCR tests and issued guidelines to try and minimize them. But for COVID-19, the two organizations somehow forgot all about PCR false-positive rates.
In research published at medRXiv, titled, “Diagnosing COVID-19 infection: the danger of over-reliance on positive test results,” the authors provided evidence that shows false-positive PCR results are common enough to impact clinical and policy decisions. 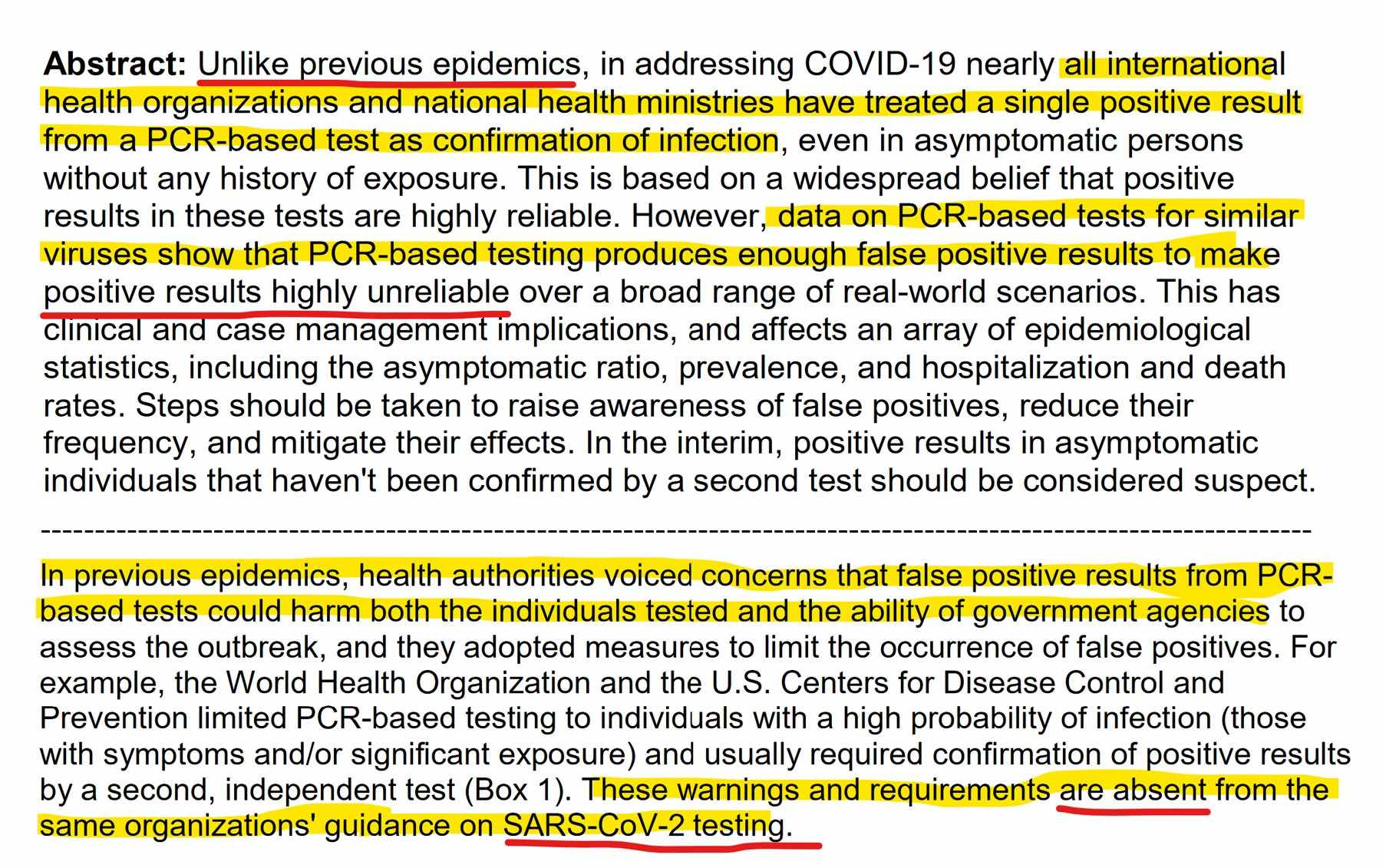
Below is a screenshot of the new guidelines released by The WHO.
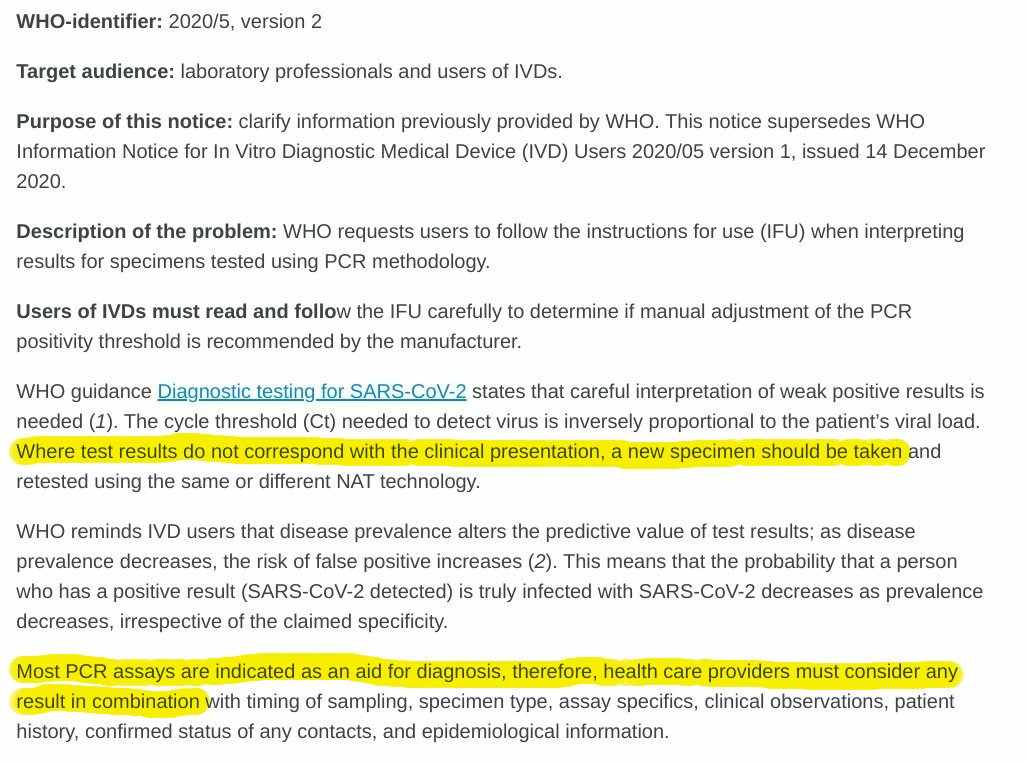
Below is the entire guidelines released by The WHO.
Nucleic acid testing (NAT) technologies that use polymerase chain reaction (PCR) for detection of SARS-CoV-2
Medical product alert
Geneva
Reading time: 1 min (370 words)
Product type: Nucleic acid testing (NAT) technologies that use polymerase chain reaction (PCR) for detection of SARS-CoV-2
Date: 13 January 2021
WHO-identifier: 2020/5, version 2
Target audience: laboratory professionals and users of IVDs.
Purpose of this notice: clarify information previously provided by WHO. This notice supersedes WHO Information Notice for In Vitro Diagnostic Medical Device (IVD) Users 2020/05 version 1, issued 14 December 2020.
Description of the problem: WHO requests users to follow the instructions for use (IFU) when interpreting results for specimens tested using PCR methodology.
Users of IVDs must read and follow the IFU carefully to determine if manual adjustment of the PCR positivity threshold is recommended by the manufacturer.
WHO guidance Diagnostic testing for SARS-CoV-2 states that careful interpretation of weak positive results is needed (1). The cycle threshold (Ct) needed to detect virus is inversely proportional to the patient’s viral load. Where test results do not correspond with the clinical presentation, a new specimen should be taken and retested using the same or different NAT technology.
WHO reminds IVD users that disease prevalence alters the predictive value of test results; as disease prevalence decreases, the risk of false positive increases (2). This means that the probability that a person who has a positive result (SARS-CoV-2 detected) is truly infected with SARS-CoV-2 decreases as prevalence decreases, irrespective of the claimed specificity.
Most PCR assays are indicated as an aid for diagnosis, therefore, health care providers must consider any result in combination with timing of sampling, specimen type, assay specifics, clinical observations, patient history, confirmed status of any contacts, and epidemiological information.
Actions to be taken by IVD users:
- Please read carefully the IFU in its entirety.
- Contact your local representative if there is any aspect of the IFU that is unclear to you.
- Check the IFU for each incoming consignment to detect any changes to the IFU.
- Provide the Ct value in the report to the requesting health care provider.
Contact person for further information:
Anita SANDS, Regulation and Prequalification, World Health Organization, e-mail: rapidalert@who.int
References:
1. Diagnostic testing for SARS-CoV-2. Geneva: World Health Organization; 2020, WHO reference number WHO/2019-nCoV/laboratory/2020.6.
2. Altman DG, Bland JM. Diagnostic tests 2: Predictive values. BMJ. 1994 Jul 9;309(6947):102. doi: 10.1136/bmj.309.6947.102.
__


Ei kommentteja:
Lähetä kommentti